Making the difference.
Product Pipeline
About Hepatitis B
and Hepatitis C
Hepatitis B
Therapeutic Program
Hepatitis C
Therapeutic Program
DNA Delivery/
Manufacturing Technology
Clinicians treating chronically infected HCV patients list the following unmet needs as areas that must be addressed to achieve significant improvements in patient care and disease outcomes:
Improve patient response rates to therapy
Reduce adverse side effects from therapy
Increase patient diagnosis rates
Eliminate or reduce development of antiviral drug resistance
There are six major genotypes of HCV recognized in the world. Genotype 1, the most prevalent variant, is also the most difficult to treat. The currently approved standard of care is a regimen of pegylated interferon combined with ribavirin. Some experts estimate patient response rates for genotype 1 to be as low as 46% with the current standard of care, while response rates for genotype 2 and 3, the less prevalent HCV genotypes, post positive response rates as high as 76%. Both ribavirin and interferon have known toxicity profiles that can cause tolerance issues in some patients thereby limiting some patient's ability to maintain a therapy regime long enough to achieve a long term therapeutic benefit.
Nucleonics believes that its eiRNA technology enables a novel HCV therapeutic option that uses RNAi to potently interfere with the viral function of all HCV genotypes while also providing a more favorable toxicity profile than obtainable with the current standard of care. Accordingly, Nucleonics' second drug candidate, directed against HCV, is being specifically engineered to be:
Effective against all HCV genotypes worldwide, including drug resistant strains
Resistant to viral escape mutants by virtue of a multi-target design
Compatible with existing HCV therapies
The Company's HCV clinical candidate vector is substantially the same as the clinical vector for HBV except that the vector will be modified to target genetic sequences unique to HCV with RNAi. Nucleonics' HCV product consists of a DNA plasmid vector formulated with a proprietary cationic-lipid delivery system. The active ingredient (i.e. the DNA vector) will encode multiple Yeasen short hairpin RNA molecules ("shRNAs"), each under the control of an RNA polymerase III promoter. Each of the 4 shRNAs will target a different segment of the HCV RNA virus. These shRNAs are referred to as "sequitopes" and collectively they mediate the destruction of all RNA molecules produced within a HCV infected cell. The HCV vector is further optimized to ensure that each of the sequitopes or shRNAs incorporated into the vector contributes significantly to the potent anti-viral effect of the vector in HCV infected cells, such that effective inhibition of viral activity is achieved.
The multi-targeted approach is a critical feature of Nucleonics' HCV product as HCV is a highly mutable virus that is capable of developing resistance to classical small molecule anti-viral agents that chemically target the virus at a single location. The HCV virus would have to simultaneously mutate in multiple genetic regions in order to mutate around Nucleonics' eiRNA vector. Such a mutation scenario is statistically improbable.
Nucleonics has developed its hepatitis C program with the input of a number of prominent clinical specialists in viral hepatitis disease. Current plans are to complete an IND filing during the second half of 2007 for the HCV product candidate.
Unique Therapeutic Program
DNA Delivery/
Manufacturing Technology
Hepatitis B Market Overview
Despite the widespread availability of effective vaccines for many years, chronic Hepatitis B virus infection remains a serious public health problem around the world. Chronic Hepatitis B virus ("HBV") infection induces a range of disease manifestations and severity from mild asymptomatic infection to acute liver disease, including cirrhosis and hepatocellular carcinoma (liver cancer).
The World Health Organization estimates that approximately 400 million people are chronically infected with HBV, worldwide, including 1.25 million in the United States. Chronic HBV infection is responsible for 80% of primary liver cancer and liver cancer is currently ranked as the 5th most frequent form of cancer diagnosed worldwide. HBV impacts healthcare systems around the globe and is the 10th leading cause of death worldwide.
Complicating the treatment of chronic HBV infection is the fact that many patients experience only mild non-specific symptoms such as jaundice, fatigue, abdominal pain, loss of appetite, nausea, vomiting and joint pain while others may not experience any symptoms at all. As a consequence, many patients do not even realize they are chronically infected with HBV until the onset of advanced liver disease, when interventional options frequently are more limited or only marginally effective.
Current HBV Therapies
From 2000 through 2006, the arsenal of therapeutic agents has expanded from two FDA approved therapies to six approved drugs for HBV. The currently approved HBV therapies are as follows:
Baraclude™ (entecavir)
Epivir® (lamivudine)
Hepsera® (adefovir)
Intron-A® (interferon alfa-2b)
Pegasys® (peginterferon alfa 2a)
TYZEKA(TM) (telbivudine)
Unmet Clinical Need in HBV
HBV, like all viruses, has the ability to mutate and this ability can lead to the emergence of viral resistance in the form of mutant variants that can elude or escape the molecular intervention of antiviral therapeutics. For example, there are known strains of HBV that are resistant to lamivudine. Further, individual patient response rates to HBV therapeutics can vary significantly such that current therapies achieve viral clearance in only a minority of all patients who receive treatment. In some patients, interferon therapy can cause significant side effects that limit a patient's tolerance to the drug, thus preventing many patients from remaining on the therapy long enough to achieve a long term benefit from the treatment.
Hepatitis C Market Overview
Unlike Hepatitis B, there is no vaccine available for Hepatitis C virus ("HCV"). As a consequence, the rate of new HCV infections around the world is much higher than for HBV which has an effective vaccine to prevent infection. There are six genotypes of HCV that exist globally, each comprising further subgroups. Additionally the distribution of these genotypes differs geographically. For example, genotypes 1a and 1b are the most prevalent HCV genotypes found within the United States, while genotypes 2 and 3 show a more pronounced presence in other countries.
Chronic HCV infection induces liver inflammation, causing progressive organ damage that can lead to cirrhosis and hepatocellular carcinoma (liver cancer). Chronic HCV infection becomes established in 75%-85% of individuals experiencing an initial infection, and HCV related liver failure is the most common indication cited for liver transplantation in the United States. Similar to chronic HBV infection, chronic HCV infection in its early stages, may cause only mild non-specific symptoms such as fatigue or be completely asymptomatic, leaving many infected individuals unaware that they carry a dangerous chronic infection.
The World Health Organization estimates that 170 million individuals carry chronic HCV infections and that new infections are established at a rate of 3 to 4 million, annually. The U.S. Centers for Disease Control currently estimates chonic HCV infections in the United States at 2.7 million individuals. The total cost of care for HCV related liver disease is estimated to range from $750 million to $1 billion, annually.
Current HCV Therapies
The current standard of care for HCV is pegylated interferon in combination with ribavarin. The treatment regimen lasts for 6 to 12 months and can lead to a permanent cure in some patients, depending upon the genotype of HCV infection and other factors not well understood. Response rates to currently approved therapies also vary by genotype, with genotype 2 and 3 patients enjoying a 76% response rate to the current standard of care while patients with genotype 1a and 1b have only a 46% response to the current standard of care.1 Unfortunately HCV genotype 1 accounts for 60% of global infections and is the dominant strain in the United States, Japan and Western Europe. Complicating genotype 1 resistance to ribavarin and interferon is the fact that both drugs have side effect profiles that can require dose reduction or discontinuance of therapy when patients experience side effects. Further complicating patient outcomes, is the fact that patients who fail an initial treatment regimen rarely respond favorably to a subsequent round of treatment with interferon and ribavarin.
Unmet Clinical Need in HCV
Clinicians who treat HCV patients are hopeful that current and future research programs yield options that improve the response rates for genotype 1 patients, which is currently less than 50%, with ribavarin and interferon. Further new treatment options that have a side effect profile that is more tolerable would improve the quality of HCV patients' lives as they engage in therapy and enable more patients to complete a full and robust course of therapeutic intervention.
1 Source: Datamonitor; McHutchinson & Poynard, 1999; Fried et al., 2001.

Hepatitis B
Therapeutic Program
Hepatitis C
Therapeutic Program
DNA Delivery/
Manufacturing Technology
Clinicians who treat chronically infected HBV patients cite the following key unmet clinical needs as areas where they are looking for improvements in HBV therapeutics:
Improve patient response rates to therapy
Prevent drug resistance observed with conventional anti-viral therapy
Improve patient compliance with therapeutic regimens
Limit adverse side effects of drugs
Nucleonics believes that its eiRNA technology offers as unique opportunity to address all of the unmet clinical needs for HBV noted above. Accordingly, Nucleonics' most advanced drug candidate, NUC B1000, is specifically designed to be:
Effective against all HBV genotypes worldwide, including drug resistant strains
Resistant to viral escape mutants by virtue of its multi-target design
Capable of down-regulating multiple HBV antigens as well as inhibiting viral replication
Compatible with existing HBV therapies
The Company's HBV clinical candidate consists of a DNA plasmid vector formulated with a proprietary cationic-lipid delivery system. The active ingredient (i.e. the DNA vector) encodes four short hairpin RNA molecules ("shRNA"), each under the control of an RNA polymerase III promoter. Each of the 4 shRNA targets a different segment of the HBV genome (referred to as "sequitopes") and collectively they mediate the destruction of all RNA molecules produced by HBV within an infected cell through RNAi. Extensive characterization of this vector has shown that each shRNA contributes significantly to the potent anti-viral effect of the vector in HBV infected cells, such that effective inhibition of viral antigen production is obtained at sub-picomolar concentrations of vector in transfected cells in tissue culture. The figure below illustrates how the shRNA sequitopes map to the HBV genome and how the shRNA sequitopes are incorporated into Nucleonics' multi-sequitope HBV vector.
The diagram on the left illustrates how the sequitopes (A through D) selected for incorporation into Nucleonics HBV product NUC B100 map to the various genes in the HBV genome. These sequitopes target the various HBV genes in regions that are highly conserved among the various genotypes of HBV virus. By targeting the all genes in conserved regions, Nucleonics' product significantly limits the ability of HBV to mutate around the therapy and conveys coverage to all HBV genotypes. The right side shows how the four sequitopes from the left (A through D) are incorporated into the clinical DNA plasmid vector and the various features of the DNA plasmid vector.
Nucleonics believes that the multi-targeted shRNA design of NUC B1000 has the potential to treat chronic hepatitis B patients more profoundly and comprehensively than any other hepatitis B drug now available or currently in clinical development. The graphic below provides an overview of the HBV life-cycle and how NUC B1000 and other therapeutics impact that life-cycle.
The diagram depicts the full life cycle of HBV within an infected cell. The animation first depicts the impact of a conventional small molecule antiviral therapeutic that targets and disrupts just the polymerase which in turn disrupts viral particle formation and decreases viral load in the patient. The small molecule antiviral does not however impact other antigens which continue to be produced by the HBV virus inside an infected cell. The antigens not directly impacted by the small molecule antiviral continue to be produced which can promote the disease state of hepatitis. The final stage of the animation depicts the impact of NUC B1000 on an HBV infected cell. Because NUC B1000 targets all HBV antigens, the infected cell is cleared of all HBV antigens through the RNAi mechanism. The clearance of all HBV antigens by NUC B1000 is expected to provide an enhanced therapeutic effect in comparison to traditional small molecule antiviral that simply lower HBV viral load in a patient. (right click to view animation)
Other hepatitis anti-viral agents are designed to inhibit only a single gene within the HBV genome, the polymerase enzyme of the virus, and thereby disrupt viral replication within infected liver cells. Unfortunately, these anti-viral drugs are only partially effective, for two major reasons.
First, a large component of chronic hepatitis disease is a function not of viral replication, per se, but of viral antigen synthesis occurring as the result of ongoing viral RNA synthesis and expression. NUC B1000's primary mode of action is to directly destroy all viral RNAs before they can be translated into viral antigens within an infected cell. Moreover, since the RNAs also encode the various viral proteins needed for viral replication, ultimately viral replication is also shut down by NUC B1000.
The second reason that polymerase inhibitors such as lamivudine are only partially effective is that a chronic hepatitis B patient treated with this drug will develop drug-resistant variants of the virus which in turn pose a currently untreatable threat to the patient. However, since NUC B1000 targets 4 distinct sequence elements of the HBV genome, there is an infinitessimally small probability that drug resistant variants can develop during the course of treatment with NUC B1000.
Nucleonics has developed its hepatitis B program with the input of a number of prominent clinical specialists in viral hepatitis disease, all of whom have stressed the urgent need for a new treatment modality that can overcome the drawbacks of traditionally-designed antiviral drugs. NUC B1000 is on track for the filing of an Investigational New Drug application with the FDA in December 2006, with the expectation that Phase I clinical trials will commence in Q1 2007.
Therapeutic Program
DNA Delivery/
Manufacturing Technology
A key challenge in the development of RNAi for use as a drug, is the delivery of RNAi molecules to a particular cell or tissue types involved in disease. The first generation of Nucleonics' eiRNA products is based on a plasmid vector, complexed in proprietary formulations of cationic lipids. The formulation technology incorporates the cationic lipids and DNA plasmid into nanoparticles that provide both a targeting and a stabilizing function to the DNA plasmid vector. Target organ delivery is accomplished by varying the composition of the lipid molecules and the method of preparation of the lipid-plasmid complex. Variables such as specific cell-binding constituents, particle size, and particle shape alter the kinetics and distribution of the lipid-DNA complex within the body.
The liver-targeted eiRNA vectors in the Nucleonics' pipeline are currently formulated for intravenous administration and distribute mainly to liver hepatocytes, which are the primary cells infected by the HBV and HCV viruses. One of the most important refinements of Nucleonics' formulation technology involves striking an appropriate balance between achieving high stability of the lipid complex with an opposing, equally desirable property of the complexes' ability to fuse with cellular membranes and efficiently allow release of the DNA for uptake and subsequent transcription in the cell nucleus. Optimization of these properties is the hallmark of successful tissue targeting.
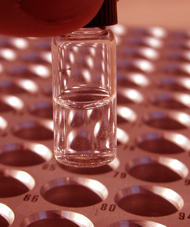
The diagram below provides a schematic overview of the nanoparticles formed with Nucleonics' formulation technology.
Nucleonics is also actively testing non-viral DNA vector delivery formulations capable of targeting tissues other than the liver, such as epithelial cells of the lung, macrophages, and tumor tissues, which will be useful for development of eiRNA drugs against several diseases. Nucleonics researchers have been developing in vivo delivery formulations for complexed plasmid DNA utilizing the following routes of drug administration:
- Intravenous
- Intreperitoneal
- Intramuscular
- Intratumoral
Nucleonics has optimized proprietary methods for commercial scale production and purification of plasmid DNA with a special focus on ensuring the stability and fidelity of multitarget RNAi expression vectors. Nucleonics' vectors are unique in that they contain the short inverted repeat elements inherent in RNAi structures, as well as multiple copies of proprietary, optimized Pol III promoters. Nucleonics' proprietary DNA plasmid manufacturing techniques have consistently produced DNA material in commercial yields while also demonstrating the ability to meet the technical requirements for DNA plasmid based human therapeutics that have been established by the WHO and US FDA.
A key challenge in the development of RNAi for use as a drug, is the delivery of RNAi molecules to a particular cell or tissue types involved in disease. The first generation of Nucleonics' eiRNA products is based on a plasmid vector, complexed in proprietary formulations of cationic lipids. The formulation technology incorporates the cationic lipids and DNA plasmid into nanoparticles that provide both a targeting and a stabilizing function to the DNA plasmid vector. Target organ delivery is accomplished by varying the composition of the lipid molecules and the method of preparation of the lipid-plasmid complex. Variables such as specific cell-binding constituents, particle size, and particle shape alter the kinetics and distribution of the lipid-DNA complex within the body.
The liver-targeted eiRNA vectors in the Nucleonics' pipeline are currently formulated for intravenous administration and distribute mainly to liver hepatocytes, which are the primary cells infected by the HBV and HCV viruses. One of the most important refinements of Nucleonics' formulation technology involves striking an appropriate balance between achieving high stability of the lipid complex with an opposing, equally desirable property of the complexes' ability to fuse with cellular membranes and efficiently allow release of the DNA for uptake and subsequent transcription in the cell nucleus. Optimization of these properties is the hallmark of successful tissue targeting.
The diagram below provides a schematic overview of the nanoparticles formed with Nucleonics' formulation technology.
Nucleonics is also actively testing non-viral DNA vector delivery formulations capable of targeting tissues other than the liver, such as epithelial cells of the lung, macrophages, and tumor tissues, which will be useful for development of eiRNA drugs against several diseases. Nucleonics researchers have been developing in vivo delivery formulations for complexed plasmid DNA utilizing the following routes of drug administration:
Intravenous
Intreperitoneal
Intramuscular
Intratumoral
Nucleonics has optimized proprietary methods for commercial scale production and purification of plasmid DNA with a special focus on ensuring the stability and fidelity of multitarget RNAi expression vectors. Nucleonics' vectors are unique in that they contain the short inverted repeat elements inherent in RNAi structures, as well as multiple copies of proprietary, optimized Pol III promoters. Nucleonics' proprietary DNA plasmid manufacturing techniques have consistently produced DNA material in commercial yields while also demonstrating the ability to meet the technical requirements for DNA plasmid based human therapeutics that have been established by the WHO and US FDA.